Ankylosing spondylitis (AS) is an autoimmune condition that causes inflammation in the spine, joints, and bones.
Ankylosing spondylitis affects women more often than previously thought. In the past, AS was believed to more commonly affect men, but newer research suggests the rates may be nearly equal between the two groups.
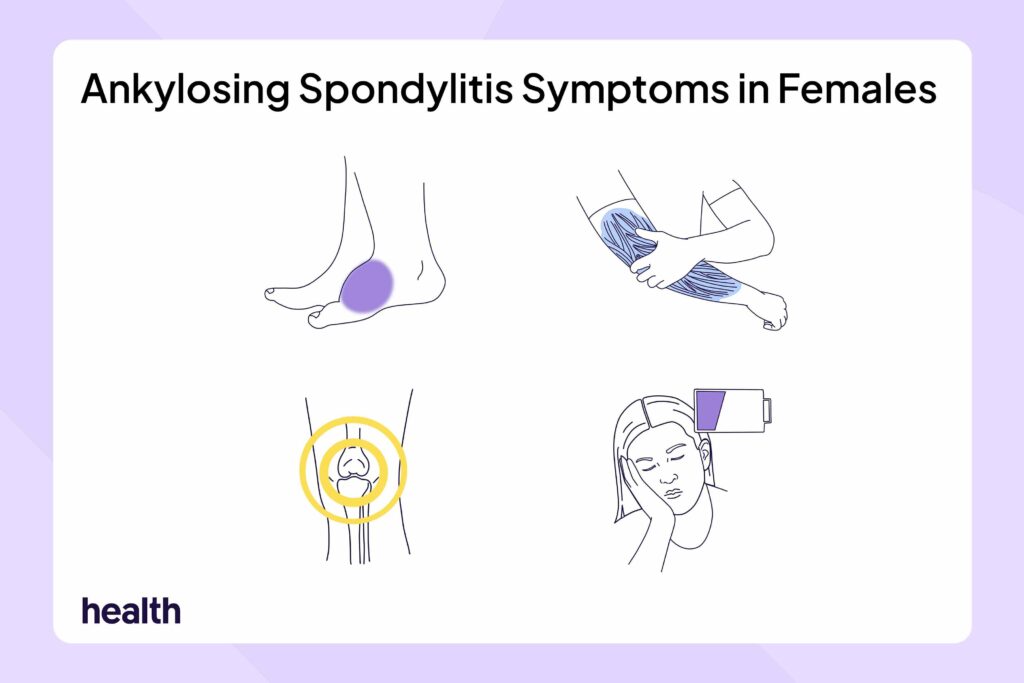
If you were assigned female at birth, AS can cause unique symptoms, making it harder to diagnose.
Design by Health
Whether you were assigned female or male at birth, the main symptoms people with ankylosing spondylitis may experience include:
- Back and spine pain
- Joint pain, swelling, and stiffness
- Fatigue
- Anterior uveitis (inflammation of the front part of the eye)
Women may experience additional AS symptoms or overlapping health conditions that affect other parts of the body beyond the spine and joints. Women with AS may be more likely to have the following:
- Dactylitis: This is swelling of an entire finger or toe. It is sometimes referred to as sausage digits. Dactylitis can be painful and make it hard to grip, walk, or use your hands.
- Enthesitis: This is pain and tenderness where tendons or ligaments attach to bone, like the back of your heel, under your foot, or around your pelvis.
- Inflammatory bowel disease (IBD): This causes inflammation of the digestive tract and includes conditions like Crohn’s disease and ulcerative colitis. You might notice ongoing stomach pain, diarrhea, or other gut problems.
- Psoriasis: This skin condition causes red, scaly patches, often on the elbows, knees, scalp, or lower back. Psoriasis may flare up alongside joint pain or stiffness.
Ankylosing spondylitis symptoms can vary quite a bit between women and men. Here are seven ways AS symptoms differ between the sexes:
1. Symptoms May Start Later and Delay Diagnosis
Research shows that women tend to develop AS symptoms at a slightly older age.
The symptoms women develop may also be harder to recognize, potentially delaying diagnosis. In fact, the time to diagnosis is longer among females. On average, it takes women nine years before being diagnosed with AS compared to about seven years for men.
2. More Widespread and Intense Pain
Instead of the typical back pain with AS, women often feel pain all over their body. The pain tends to be intense. Women may also develop more enthesitis, longer-lasting morning stiffness, and extreme fatigue.
Researchers believe this occurs partly because women have more pain receptors in their bodies and may process pain signals differently.
3. Different Joints Are Affected
AS is known for affecting the spine. But in females, the condition often develops in the peripheral joints, like the knees, ankles, elbows, or wrists.
4. Less Spine Damage on X-Rays
Men with AS are more likely to develop severe spinal fusion over time, where the vertebrae grow together and lose flexibility. This is sometimes called “bamboo spine” and can be detected on X-rays.
At the time of diagnosis, women with AS tend to show less spine damage on X-rays. They’re also less likely to develop bamboo spine over time.
5. Symptoms May Be Harder To Manage
Women may not respond as well to certain AS treatments, especially tumor necrosis factor (TNF) inhibitors. TNF inhibitors are biologic medications used to decrease inflammation and improve symptoms. These medications may not work as well or may stop working sooner in women, which can make symptom management more challenging.
6. IBD Is More Common
Women with AS are more likely to develop inflammatory bowel disease. This means they may be more likely to develop symptoms of Crohn’s disease or ulcerative colitis, two types of IBD. These symptoms can include diarrhea, changes in bowel movements, stomach pain, and fatigue.
7. Hormones Can Affect Symptoms
Hormonal changes, like those that occur during menstruation, pregnancy, or menopause, may affect how AS symptoms develop and how intense they feel.
Women often report flare-ups around their period, and some research suggests that estrogen may play a role in how the body handles inflammation. Lower estrogen levels, such as during menopause, might lead to increased disease activity or more noticeable joint pain. However, research is still ongoing to understand this effect.
While females have to consider symptoms specific to them, they may also have to consider what impact ankylosing spondylitis might have on their fertility and pregnancy.
Does AS Affect Your Ability To Get Pregnant?
There’s currently no strong evidence that having AS affects your ability to get pregnant. However, some research shows that women with AS have lower levels of anti-Müllerian hormone, which can mean fewer eggs available for pregnancy. But more research is needed to fully understand this link.
It’s also possible that certain medications used to treat AS, like steroids and non-steroidal anti-inflammatory drugs (NSAIDs), can reduce fertility. Fertility may also be affected by inflammation, hormone changes, and emotional stress. If you have AS and are planning to start a family, talk to your rheumatologist and a fertility specialist early on. They can help you find a plan that supports both your AS and your reproductive goals.
Do AS Symptoms Change During Pregnancy?
You may feel better during pregnancy. Or, symptoms might worsen, particularly in the second and third trimesters. This could happen if you stop taking your medications or due to the physical changes your body undergoes.
If AS becomes more active during pregnancy, you might have a higher risk of complications like gestational diabetes, preeclampsia, and early delivery. Yet, many people with AS can have healthy pregnancies. Having a care team and mental health support can help you manage the condition and your health through pregnancy and beyond.
These are two main factors that can lead to many females waiting longer before receiving an accurate ankylosing spondylitis diagnosis:
- AS symptoms in females don’t always match the expected pattern. The atypical symptoms can lead to delayed or incorrect diagnosis. For example, joint pain in the arms and legs or widespread body pain may prompt doctors to first consider other conditions besides AS. Since AS was historically thought to mainly affect males, some doctors may not immediately think to test for it in females.
- X-rays might not show the typical spine changes doctors look for when diagnosing AS. This can lead to the condition being overlooked or mistaken for other health issues like fibromyalgia. And because females often experience overlapping health conditions, like IBD and psoriasis, it can be even more challenging for doctors to identify AS as the underlying cause.
Females often experience ankylosing spondylitis (AS) differently than men. Women tend to have more widespread pain, increased fatigue, and pain in the arm and leg joints. Women also typically have fewer spine-focused symptoms, with AS spine damage not visible on X-rays like it is for many men. Because symptoms may not follow the typical pattern, females often face delays before getting an accurate diagnosis.