Tachycardia is the medical term for a heart rate over 100 beats per minute (BPM). It can be a sign of emotional distress or anxiety, anemia (low levels of iron in the blood), infections, dehydration, or medical emergencies like heart failure or heart attack.
Seeking care for this condition is important, as it can raise your risk of cardiovascular (heart-related) complications.
A healthy adult’s heart beats 60-100 times a minute, and it’s normal for your heartbeat to rise with physical activity, stress, or emotional reactions. However, tachycardia causes your heart to beat more than 100 times a minute at rest.
If you consistently have tachycardia or have other concerns about your heart health, you should reach out to a healthcare provider.
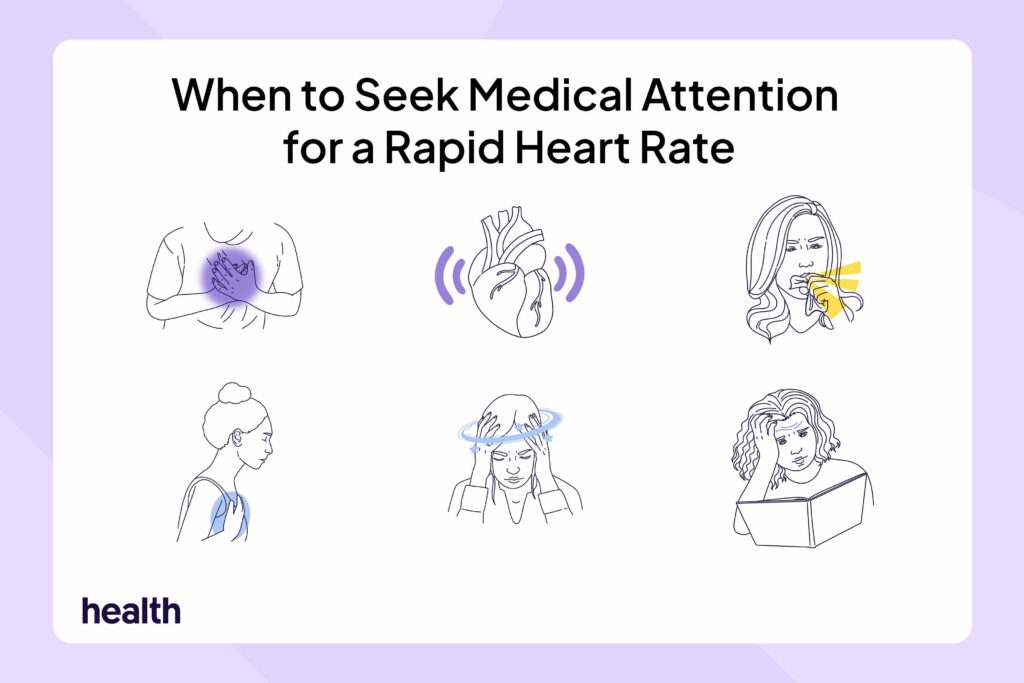
Having tachycardia alongside any of these symptoms requires medical care:
- Palpitations (irregular, fluttering, or out-of-rhythm heartbeats)
- Dyspnea (trouble breathing)
- Persistent cough
- Lightheadedness
- Fatigue
- Swelling, specifically in the feet, hands, fingers, legs, and ankles
- Chest pain
- Confusion (memory loss, disorientation, and difficulty understanding)
- Nausea and vomiting
Seek immediate emergency care if you or a loved one has serious symptoms or loses consciousness. If a person loses consciousness while waiting for emergency services, check their breathing. If they aren’t breathing, perform cardiopulmonary resuscitation (CPR) and, if available, use an AED. An AED is a medical device that can check the heart’s rhythm and deliver a shock to help restore a normal heart rhythm.
At the emergency room (ER), the goal of the care team is to stabilize your heart rate and prevent complications. They’ll take your medical history, ask about past cardiac events, and find out if you take any medications to determine the cause of the tachycardia. They’ll also perform tests, which may include:
- Electrocardiogram (ECG/EKG): This measures your heart’s activity. It uses electrodes (small sensors that stick to your arms, legs, and chest) attached to wires that connect to the EKG. This can show if your fast heartbeat is from tachycardia.
- Echocardiogram (echo): This uses sound waves to create images of the heart’s structure and can help determine if your heart is working properly. If your heart is working harder than normal to function, this could be due to tachycardia.
- Chest X-ray: This takes an image of your chest, including the lungs, heart, large arteries, ribs, and diaphragm (the main muscle responsible for breathing). This can show if your heart is bigger than it should be or if you have lung problems that may be related to tachycardia.
- Cardiac magnetic resonance imaging (cardiac MRI): This makes detailed images of the heart muscles. It can show if there’s any scarring or damage to the heart.
- Coronary angiogram: This uses an injected dye and X-rays to check whether blood is flowing properly through the heart and detect any blockages that may be caused by tachycardia.
- Pulse oximetry: Tachycardia can affect oxygen levels in your blood. This test measures your blood oxygen levels.
- Blood tests: This may include a complete blood count (CBC), which is a group of blood tests that measure the number and size of your blood cells. Conditions like anemia can cause tachycardia by making your heart beat faster. A CBC can help find anemia and determine whether it might be causing your fast heartbeat.
Specific treatments in the ER depend on the cause and may include:
- Vagal maneuvers: These physical maneuvers slow the heart rate. They include coughing, blowing out of your nose while pinching it shut, or applying an icepack to your face.
- Medications: In the ER, you may receive intravenous (IV) medications, which are delivered through the veins, to help slow your heart rate. These may include beta-blockers, calcium channel antagonists, or Lanoxin (digoxin), a medication used to treat heart failure.
- Cardioversion: This uses electrodes to deliver electrical currents to the heart, helping it return to a normal rhythm.
- Catheter ablation: In this test, a healthcare provider inserts a catheter (a flexible tube) into a blood vessel (a tube that carries blood), often in the groin. They then guide the catheter to the heart and use heat or cold energy to scar the heart tissue, changing activity patterns.
- Defibrillation: In severe cases, healthcare providers may use a defibrillator to apply electrical charges to restore the heartbeat.
Preventing future tachycardia episodes can vary depending on the person, the underlying cause, and the type of tachycardia. Typically, you and your doctor will come up with a plan to manage an elevated heart rate and prevent complications. This may involve taking medication, along with incorporating certain lifestyle changes that keep your heart healthy.
Certain types of tachycardia can be dangerous and should be diagnosed and managed by a cardiologist. A cardiologist is a doctor who specializes in treating and diagnosing heart and blood vessel conditions.
Eat Well
Making dietary changes can help support a healthy heart. You can do this if you:
- Choose foods high in fiber, vitamins, and minerals, such as whole grains, fruit, and vegetables
- Incorporate healthy proteins and fats, such as low-fat dairy, skinless chicken, fish, nuts, and beans
- Limit trans fats, saturated fats, sugar, salt, and processed foods
Get Exercise
In general, getting enough physical activity helps support heart health and reduces your risk of heart disease. Risk factors include high cholesterol levels (fat levels in your blood), high blood pressure, or being a higher weight than discussed with your provider. The recommended amount of weekly exercise includes at least 150 minutes of light to moderate activity.
Your doctor may recommend avoiding strenuous exercise or competitive sports if you have certain types of tachycardia.
Lifestyle Changes
Certain lifestyle changes can help keep your heart healthy and possibly lower your risk of having tachycardia. You can lower your risk if you:
- Avoid smoking and any recreational drugs
- Stay hydrated
- Limit or stop alcohol use
- Avoid tachycardia triggers, such as caffeine or stimulants
- Get enough sleep (7-8 hours a night for adults) with consistent bed and wake-up times
Manage Stress
Stress and anxiety affect heart health and can increase heart rate. Stress management strategies, such as meditation, yoga, or relaxing activities, may help. Don’t be afraid to seek out support from family, loved ones, and friends. If you’re struggling, seek professional counseling.
Weight Management
Being a higher weight than discussed with your provider can raise your risk of heart disease, high cholesterol, diabetes, and other chronic (long-term) conditions. If you’re experiencing obesity or are overweight, a 5-10% reduction in weight can significantly lower these risks. Consider talking to your healthcare provider about weight management options.
Treating Underlying Conditions
Preventing elevated heart rate and heart complications can also mean managing risk factors and underlying conditions. This may mean taking medications and making lifestyle changes to manage type 2 diabetes, high cholesterol, and high blood pressure.
Taking Medications
If you have recurring tachycardia due to a heart arrhythmia (irregular heartbeat) or other heart conditions, your healthcare provider may prescribe medications to control heart rate, including:
- Beta-blockers
- Calcium channel blockers
- Ivabradine, a medication used for heart failure
- Antiarrhythmic medications, which are used to treat and prevent heart rhythm changes
Medical Procedures
If other methods don’t work, several medical treatments can help manage your heartbeat:
- Pacemaker: This is an implanted electrical device that uses electricity to control the heart’s rhythm.
- Implantable defibrillator: These are devices that are placed under the skin. They detect irregular heartbeats and send electrical currents to the heart to regulate activity.
- Maze procedure: This is a surgery where the surgeon creates scar tissue on the heart to help treat certain arrhythmia conditions.
Medical Monitoring and Advice
If you often experience a racing heartbeat or other heart health symptoms, it’s important to seek care and follow your provider’s advice. They’ll show you how to monitor your heart activity. Let them know if you’re making any lifestyle changes, or if medications you’re taking aren’t working or are causing side effects.
A rapid heart rate at rest is called tachycardia. It can be caused by everything from dehydration or emotional distress to serious conditions like heart failure.
If you regularly experience tachycardia or other concerning heart symptoms, let your healthcare provider know. Racing or irregular heartbeat with chest pains, loss of consciousness, confusion, and breathing difficulties are signs you need emergency help.